Gut Health Might Be the Secret to Your Exercise Motivation
What if the key to staying motivated at the gym — or even just lacing up your running shoes — has nothing to do with willpower but your gut?
Emerging research suggests that the trillions of microbes living in your digestive system could play a surprising role in how much you enjoy (or dread) physical activity. Let’s explore the science and what it means to you.
The Study: Gut Microbes and Exercise Motivation
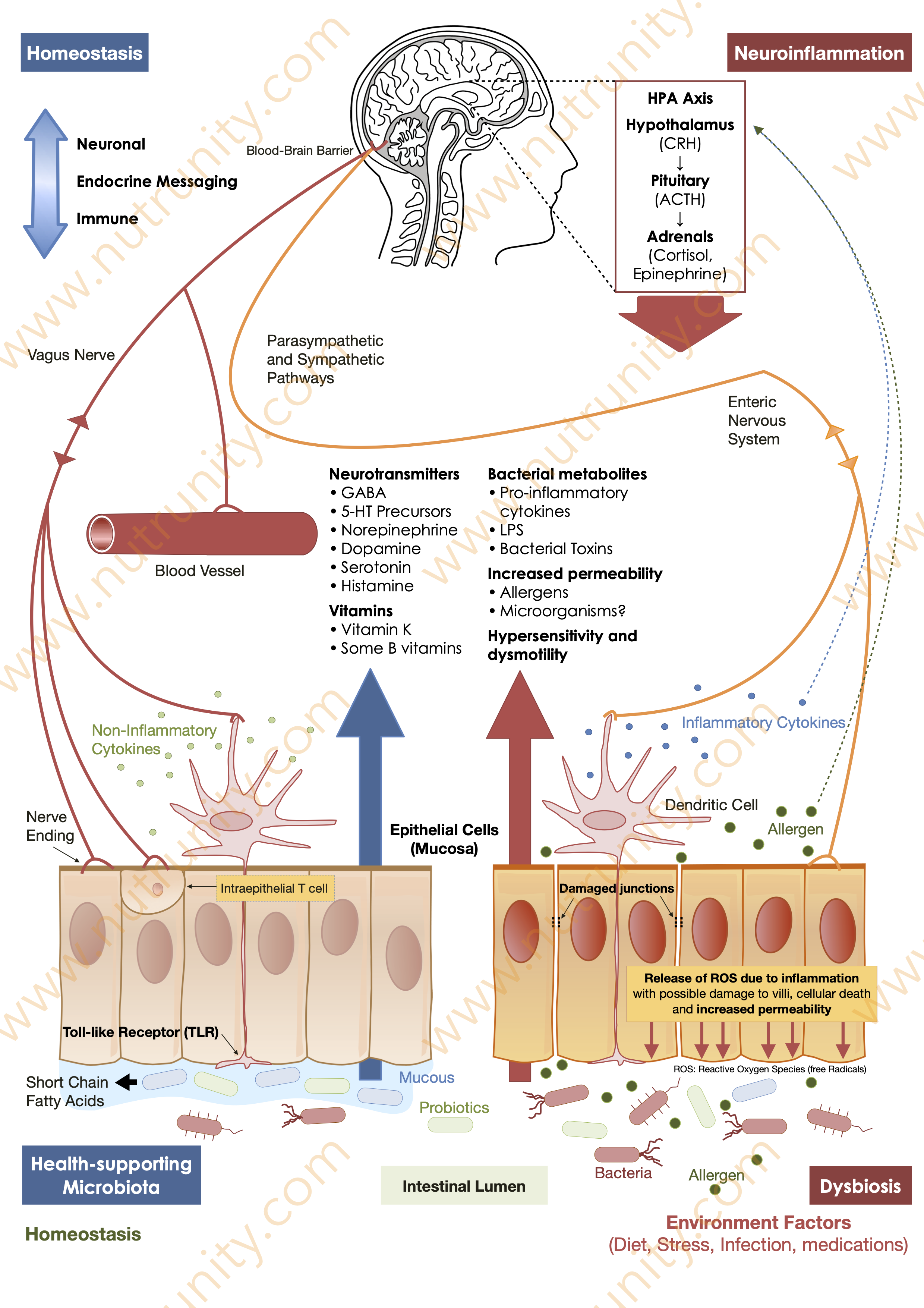
A groundbreaking animal study has revealed a fascinating connection between gut health and exercise motivation. While this research was conducted on animals, human studies have also shown that the gut microbiome plays a critical role in our health and behaviour. For example, research on physical activity has demonstrated that exercise can increase gut microbial diversity and release feel-good neurotransmitters — linked to better physical and mental performance. However, it was also noted that extreme exercising harms the gut via the stress response (HPA axis hyperactivation).
The Gut-Brain Connection: Dopamine’s Role
So, how exactly does your gut influence your desire to exercise?
The answer lies in the gut-brain axis, a complex communication network between your digestive system and brain. In humans, specific gut microbes have been shown to influence the production of dopamine, a neurotransmitter responsible for feelings of pleasure, reward, and motivation.
Low or imbalanced dopamine levels can lead to a lack of drive for physical activity. It can even contribute to conditions like major depressive disorder. This connection might explain why some people struggle to stick to a workout routine, no matter how much they want to.
What This Means for Humans
Human research supports the idea that gut health can influence behaviour and motivation. Studies have shown that probiotics and dietary changes can improve mood and cognitive function. This is thought to occur through their effects on the gut-brain axis. This is also an important reason why certain probiotics (and, to some extent, prebiotics) are also called psychobiotics.
Researchers have also found that omega-3 fatty acids, which support brain health, can enhance dopamine function. This finding opens the door to potential exercise-motivating strategies. However, the real takeaway is more straightforward: taking care of your gut health could be a game-changer for your fitness journey.
Dopamine Management
Dopamine is having a moment in the health and wellness world. Experts like Dr. Andrew Huberman have highlighted the importance of dopamine management for improving mental well-being, sleep, and even social health. As people begin to reduce their reliance on quick dopamine hits from screens and social media, there’s a growing interest in natural ways to increase this important neurotransmitter naturally.
The gut-brain axis is at the forefront of this movement, with researchers and health optimisers exploring how diet, probiotics, and lifestyle changes can influence mental and physical performance.
Actionable Takeaways: How to Optimise Your Gut for Better Motivation
Feed Your Microbes:
This sounds quite scary. However, a fibre-rich diet, fermented foods, and polyphenols (found in berries, nuts, and green tea) can promote a healthy gut microbiome. Be aware that fermented are very high in histamine and may be involved in several conditions, including transient insomnia (histamine is an excitatory neurotransmitter).
Consider Probiotics:
Specific strains of probiotics, such as Lactobacillus and Bifidobacterium, have been linked to improved gut health and mental well-being. But they are not the only ones. For example, Akkermansia muciniphila (a Gram-negative anaerobic mucus-layer-degrading bacterium) is key to increased intestinal impermeability, often found in low levels in professional athletes).
Limit Antibiotics:
While sometimes necessary, overusing antibiotics can disrupt the gut microbiome. Always use them under medical supervision. If antibiotics are available over the counter in your country, the recommendation is still to consult your doctor and complete the full course (any disruption and overuse of antibiotics is the key factor in increased drug-resistance bacteria and untreatable infections).
Maximise Fatty Acids Intake:
Omega-3 fatty acids in fatty fish, flaxseeds, pistachios and walnuts may support dopamine production and brain health.
Detox from Cheap Dopamine:
Reduce reliance on quick dopamine hits from screens and social media. Instead, seek natural rewards like exercise, social interaction, and hobbies.
Prioritise Sleep.
Chronic lack of sleep directly impacts gut health, microbial diversity, and the release of certain neurotransmitters, such as tryptophan, serotonin, and dopamine.
Manage Stress.
Chronic stress reduces digestive capabilities and microbial diversity. Meditation, yoga, and daily walks (including forest bathing) can positively impact your gut health.
Keep Hydrated.
While no one agrees on how much water we should be drinking in a day, dehydration slows down gut motility (the colon is the site of water reabsorption, the more dehydrated you are the greater the risk of constipation). Adding a few drops of electrolytes to your water can help you keep mineral levels in top shape, often lost with every cup of coffee and exercising (and stress).
Exercise Strategically.
Historically, humans had to forage or hunt for their food, continuing their night fast and “operating” with fuel provided by the body under the effect of the stress hormones (cortisol), until they ate something. For this reason, science shows that morning exercise has a greater impact compared to evening sessions, including on the gut microbiome diversity.
Detox from “Cheap” Dopamine.
Reduce the time you spend on using screens and social media. Seek natural rewards like exerciswe or hobbies.
Track Your Progress.
Use a journal or app to monitor how dietary changes affect your energy, mood, and workour consistencey.
Avoid UPFs (ultra-processed manufactured food products) and Test for Food Intolerances and Allergies if you notice symptoms occuring after eating certain foods. Keep a food diary if necessary to keep track of what you eat and the symptoms. You may also note that some symptoms are not consistant. This is because they may appear after a certain threshold.
While manufacturers would love for you to be addicted to their products, research undeniably linked those to a myriad of health conditions, increased inflammation and poorer cognition. Additionally, these products harm your gut microbiome. Opt for whole, minimally processed foods to maintain microbial harmony.
The Future of Fitness: Gut Health as a Motivator
As research into the gut-brain axis continues, the idea of using gut health to improve exercise motivation is no longer science fiction. Whether through personalised nutrition, targeted supplements, or lifestyle changes, the key to unlocking your fitness potential might be in your gut.
So, the next time you struggle to get off the couch, remember that your microbiome could be your secret weapon. Feed it well, and it might reward you with the motivation you need to crush your goals.
References
Benedict, C. Vogel, H. Jonas, W. et al. (2016). Gut microbiota and glucometabolic alterations in response to recurrent partial sleep deprivation in normal-weight young individuals. Molecular Metabolism. 5(12), pp. 1175-1186. doi:10.1016/j.molmet.2016.10.003
Clarke, SF. Murphy, EF. O’Sullivan, O. et al. (2014). Exercise and associated dietary extremes impact on gut microbial diversity. Gut. 63(12), pp. 1838-1839. doi:10.1136/gutjnl-2014-307305
Frazier, TH. DiBaise, JK. McClain, CJ. (2011). Gut microbiota, intestinal permeability, obesity-induced inflammation, and liver injury. Journal of Parenteral and Enteral Nutrition. 35(5 Suppl), 14S-20S. doi:10.1177/0148607111413772
Geurts, L. Neyrinck, AM. Delzenne, NM. et al. (2014). Gut microbiota controls adipose tissue expansion, gut barrier and glucose metabolism: novel insights into molecular targets and interventions using prebiotics. Beneficial Microbes. 5(1), pp. 3-17. doi:10.3920/BM2012.0065
Jernberg, C. Löfmark, S. Edlund, C. et al. (2007). Long-term ecological impacts of antibiotic administration on the human intestinal microbiota. ISME Journal. 1(1), pp. 56-66. doi:10.1038/ismej.2007.3
Jin, LH. Fang, ZP. Fan, MJ. et al. (2019). Bile-ology: from bench to bedside. Journal of Zhejiang University Science B. 20(5), pp. 414-427. doi:10.1631/jzus.B1900158
Karl, JP. Hatch, AM. Arcidiacono, SM. et al. (2018). Effects of psychological, environmental and physical stressors on the gut microbiota. Frontiers in Microbiology. 9, 2013. doi:10.3389/fmicb.2018.02013
Katterman, SN. Kleinman, BM. Hood, MM. et al. (2014). Mindfulness meditation as an intervention for binge eating, emotional eating, and weight loss: A systematic review. Eating Behavior. 15(2), pp. 197-204. doi:10.1016/j.eatbeh.2014.01.005
Le Chatelier, E. Nielsen, T. Qin, J. et al. (2013). Richness of human gut microbiome correlates with metabolic markers. Nature. 500(7464), pp. 541-546. doi:10.1038/nature12506. PMID: 23985870.
Messaoudi, M. Lalonde, R. Violle, N. et al. (2011). Assessment of psychotropic-like properties of a probiotic formulation (Lactobacillus helveticus R0052 and Bifidobacterium longum R0175) in rats and human subjects. British Journal of Nutrition. 105(5), pp. 755-64. doi: 10.1017/S0007114510004319
Molinaro, F. Paschetta, E. Cassader, M. et al. (2012) . Probiotics, prebiotics, energy balance, and obesity: mechanistic insights and therapeutic implications. Gastroenterology Clinics of North America. 41(4), pp. 843-854. doi:10.1016/j.gtc.2012.08.009
Robertson, CL. Ishibashi, K. Mandelkern, MA. et al. (2015). Striatal D1- and D2-type dopamine receptors are linked to motor response inhibition in human subjects. The Journal of Neuroscience. 35(15), pp. 5990 –5997
Sekirov, I. Russell, SL. Antunes, LC. et al. (2010). Gut microbiota in health and disease. Physiological Reviews. 90(3), pp. 859-904. doi:10.1152/physrev.00045.2009
Selhub, EM. Logan, AC. Bested, AC. (2014). Fermented foods, microbiota, and mental health: Ancient practice meets nutritional psychiatry. Journal of Physiological Anthropology. 33(1), 2. doi:10.1186/1880-6805-33-2
Shen, J. Obin, MS. Zhao, L. (2013). The gut microbiota, obesity and insulin resistance. Molecular Aspects of Medicine. 34(1), pp. 39-58. doi:10.1016/j.mam.2012.11.001
Sommer, F., Bäckhed, F. (2013). The gut microbiota — masters of host development and physiology. Nature Reviews Microbiology. 11, pp. 227–238. doi:10.1038/nrmicro2974
Sublette, ME. Ellis, SP. Geant, AL. et al. (2011). Meta-analysis of the effects of eicosapentaenoic acid (EPA) in clinical trials in depression. Journal of Clinical Psychiatry. 72(12), pp. 1577-1584. doi:10.4088/JCP.10m06634
Valles-Colomer, M. Falony, G. Darzi, Y. et al. (2019). The neuroactive potential of the human gut microbiota in quality of life and depression. Nature Microbiology. 4(4), pp. 623-632. doi:10.1038/s41564-018-0337-x
Volkow, ND. Wang, GJ. Telang, F. et al. (2008). Dopamine increases in striatum do not elicit craving in cocaine abusers unless they are coupled with cocaine cues. Neuroimage. 39(3), pp. 1266-1273. doi: 10.1016/j.neuroimage.2007.09.059
Watso, JC. Farquhar, WB. (2019). Hydration status and cardiovascular function. Nutrients. 11(8), 1866. doi:10.3390/nu11081866
Wiley, B. Penney, NC. Cronin, O. et al. (2014). The microbiome of professional athletes differs from that of more sedentary subjects on composition and particularly at the functional metabolic level. Gut. 67(40), pp. 625-633. doi:10.1136/gutjnl-2016-313627
Zinöcker, MK. Lindseth, IA. (2018). The Western diet-microbiome-host interaction and its role in metabolic disease. Nutrients. 10(3), 365. doi:10.3390/nu10030365